Clinical Research
(CR-042) Assessment of Wound Surface Area Measurements Using Clinically Validated AI-based Technology and Manual Evaluation Methods and Impact on Debridement Codes Billing and Reimbursement Cost
Friday, April 28, 2023
7:15 PM - 8:30 PM East Coast USA Time
Misael C. Alonso, MD – Physician, Internal Medicine, Abrazo West Campus; Robert D. J. Fraser, RN, WCC – Director Clinical Success, Clinical Success, Western University; Jose L. Ramirez Garcia Luna, PhD – Researcher, Research department, University of Montreal; David Mannion, BA – Director Marketing Development, Marketing, Swift Medical Inc.
Introduction: Manual methods overestimate wound dimensions by assuming a rectilinear shape of all wounds.1,2,3 This quality improvement study investigated the discrepancy in wound area measurements and the associated factors using different wound care assessment methods in a real-world environment. A comparison was made using an AI-based wound care application (WCA) vs. traditional paper ruler (TPR) methods. The study also compared the proportion of debridement codes submitted for reimbursement and associated billing costs by the assessment method.
Methods: In May 2022, a clinician at an outpatient clinic in the US measured the width and length of 177 wounds of 56 patients using the TPR and WCA. WCA automatically calculated the wound area measurement using the traced wound dimensions. As for the TPR, the width X length formula was used to calculate wound areas for the same wounds. The total cost of the wound care debridement was calculated for both methods using the reported CPT® billing codes 97597, 97598 and 11042-11047 based on 20 cm2.
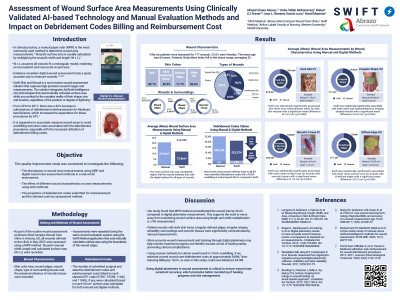
Results: The paired student-t test showed a significant difference between the average wound surface area calculation using the TPR compared to WCA technology (20.20 vs. 12.81, P=0.025, respectively).
A two-way ANOVA test found that wounds with dark skin tone using WCA were associated with a statistically significantly lower mean difference of (12.4 cm2) than a dark skin tone using the TPR method p< 0.008 (95% 3.3-21.54). Moreover, ill-defined edges, irregular shapes, surrounding unhealthy tissues and necrotic tissues using WCA were statistically significantly associated with lower mean differences in wound area measurements of 8.2 cm2 (P=0.040), 6.8 cm2 (p=0.045), 13.1 cm2 (p=0.036), and 7.6 cm2 (p=0.043), respectively, than TPR method.
The total billing cost with manual area measurement was $25,246 for 321 debridement codes submitted compared to $22,574 for 239 codes using WCA, an overbilling of $2,672.
Discussion: This inaccuracy is associated with dark skin tone wounds, irregular-defined edges, irregular shapes, unhealthy surroundings and necrotic tissues. This significant variation in wound area measurements using manual methods leads to 25.5% more submitted debridement codes with an overbilling of 10.6%.
Methods: In May 2022, a clinician at an outpatient clinic in the US measured the width and length of 177 wounds of 56 patients using the TPR and WCA. WCA automatically calculated the wound area measurement using the traced wound dimensions. As for the TPR, the width X length formula was used to calculate wound areas for the same wounds. The total cost of the wound care debridement was calculated for both methods using the reported CPT® billing codes 97597, 97598 and 11042-11047 based on 20 cm2.
Results: The paired student-t test showed a significant difference between the average wound surface area calculation using the TPR compared to WCA technology (20.20 vs. 12.81, P=0.025, respectively).
A two-way ANOVA test found that wounds with dark skin tone using WCA were associated with a statistically significantly lower mean difference of (12.4 cm2) than a dark skin tone using the TPR method p< 0.008 (95% 3.3-21.54). Moreover, ill-defined edges, irregular shapes, surrounding unhealthy tissues and necrotic tissues using WCA were statistically significantly associated with lower mean differences in wound area measurements of 8.2 cm2 (P=0.040), 6.8 cm2 (p=0.045), 13.1 cm2 (p=0.036), and 7.6 cm2 (p=0.043), respectively, than TPR method.
The total billing cost with manual area measurement was $25,246 for 321 debridement codes submitted compared to $22,574 for 239 codes using WCA, an overbilling of $2,672.
Discussion: This inaccuracy is associated with dark skin tone wounds, irregular-defined edges, irregular shapes, unhealthy surroundings and necrotic tissues. This significant variation in wound area measurements using manual methods leads to 25.5% more submitted debridement codes with an overbilling of 10.6%.

.png)