Clinical Research
(CR-050(GR-004)) Enhanced skin assessment to equitably detect early tissue damage and pressure injuries
Friday, April 28, 2023
2:15 PM - 3:15 PM East Coast USA Time
Jo Ann Otts, DNP, RN, NEA-BC, CENP – Assistant Professor, College of Nursing, University of South Alabama; Madhuri Mulekar, PhD – Professor, Mathematics and Statistics, University of South Alabama
Introduction:
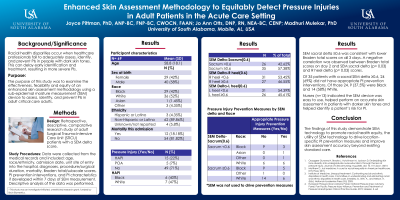
Health disparities occur when healthcare professionals fail to accurately assess skin for injury in people with darker skin color. The purpose of this study was to examine the effectiveness, feasibility, and equity of an enhanced skin assessment methodology using sub-epidermal moisture (SEM) device to assess, identify and prevent pressure injuries (PI) in critical care adults.
Methods: This was a retrospective, descriptive, comparative study. Data were collected through medical record review of adult Surgical Trauma Intensive Care Unit patients who had a SEM delta score. Data included: patient demographics, clinical information, Braden total/subscale scores, PI prevention interventions, and PI presence if developed within 7 days of SEM measurement. A web-based survey was administered to nurses who used the SEM device. Descriptive analysis of data was performed; to compare groups, one-sided t-test was performed.
Results: The study included 69 subjects; mean age 58.8 ± 18.1 years. The majority of subjects (40, 58%) were male, 29 (42%) were Black, 36 (52%) were White, and 3 (4.35%) were Other. Of the 69 subjects, 15 (23%) developed a HAPI, while 46 (70%) had no PI and 5 (7%) had a PI present on admission (POA). There were 35 (57%) subjects who had a sacral SEM delta ≥0.6, 14 (40%) were Black and 3 (21%) developed a HAPI. Nine (82%) subjects with a sacral SEM delta of ≥0.6 developed a HAPI, compared to those with SEM delta < 0.6 (2, 18%) (p= 0.048). All subjects who developed a HAPI had lower total Braden scores on days 2 (p= 0.0497) and 3 (p= 0.0337). Of those subjects with a sacral SEM delta of ≥0.6, 24 (62%) did not have appropriate HAPI prevention interventions documented. Nurses in the study (n=13) indicated the SEM device was easy to use, helped perform an accurate skin assessment in patients with darker skin tones and helped identify a patient’s risk for PI.
Discussion: This study's findings inform healthcare professionals of the clinical utility of implementing SEM technology to reduce racial health disparities, enhance appropriate PI prevention interventions, and improve nurse skin assessment accuracy beyond existing standards of PI care.
Health disparities occur when healthcare professionals fail to accurately assess skin for injury in people with darker skin color. The purpose of this study was to examine the effectiveness, feasibility, and equity of an enhanced skin assessment methodology using sub-epidermal moisture (SEM) device to assess, identify and prevent pressure injuries (PI) in critical care adults.
Methods: This was a retrospective, descriptive, comparative study. Data were collected through medical record review of adult Surgical Trauma Intensive Care Unit patients who had a SEM delta score. Data included: patient demographics, clinical information, Braden total/subscale scores, PI prevention interventions, and PI presence if developed within 7 days of SEM measurement. A web-based survey was administered to nurses who used the SEM device. Descriptive analysis of data was performed; to compare groups, one-sided t-test was performed.
Results: The study included 69 subjects; mean age 58.8 ± 18.1 years. The majority of subjects (40, 58%) were male, 29 (42%) were Black, 36 (52%) were White, and 3 (4.35%) were Other. Of the 69 subjects, 15 (23%) developed a HAPI, while 46 (70%) had no PI and 5 (7%) had a PI present on admission (POA). There were 35 (57%) subjects who had a sacral SEM delta ≥0.6, 14 (40%) were Black and 3 (21%) developed a HAPI. Nine (82%) subjects with a sacral SEM delta of ≥0.6 developed a HAPI, compared to those with SEM delta < 0.6 (2, 18%) (p= 0.048). All subjects who developed a HAPI had lower total Braden scores on days 2 (p= 0.0497) and 3 (p= 0.0337). Of those subjects with a sacral SEM delta of ≥0.6, 24 (62%) did not have appropriate HAPI prevention interventions documented. Nurses in the study (n=13) indicated the SEM device was easy to use, helped perform an accurate skin assessment in patients with darker skin tones and helped identify a patient’s risk for PI.
Discussion: This study's findings inform healthcare professionals of the clinical utility of implementing SEM technology to reduce racial health disparities, enhance appropriate PI prevention interventions, and improve nurse skin assessment accuracy beyond existing standards of PI care.

.png)
