Clinical Research
(CR-053) A pilot randomized clinical trial on the use of a novel polylactic acid dermal matrix for diabetic foot ulcer closure
Friday, April 28, 2023
7:15 PM - 8:30 PM East Coast USA Time
Brock Liden, DPM; Christian Planck, CEO; Max Froehlich, MD; Darren Doerr, MBA
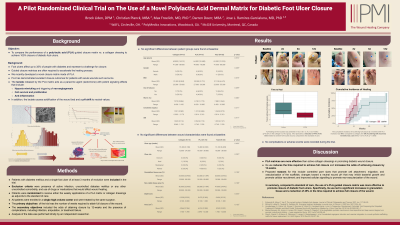
Introduction: Foot ulcers affect up to 35% of people with diabetes and represent a challenge for closure. Thus, guided closure matrices are often required to accelerate the healing process. Recently, a novel closure matrix made of polylactic acid (PLA) was developed. This material has demonstrated excellent closure outcomes for patients with acute wounds such as burns. Therefore, the objective of this study was to compare the time needed to achieve 100% closure of diabetic foot ulcers using this matrix compared to collagen dressings.
Methods: Patients with diabetes mellitus and a single foot ulcer of at least 3 months of evolution were randomized to receive either the weekly applications of a PLA matrix or collagen dressings as adjuncts to the standard of care. The wound size, the percentage of granulation tissue area, the number of weeks required to attain full closure, and the presence of complications, including infection, amputation, or treatment failure, were recorded. All patients were enrolled in a single high-volume center and were treated by the same surgeon. Analysis of the data was performed blindly by an independent researcher.
Results: A total of 28 patients were enrolled in the study (16 received PLA matrices and 12 collagen dressings). At baseline, the Hb1c, ABI, wound age, the percentage area of granulation tissue, and wound size was similar between the patient groups. All patients were followed until wound closure was attained. Granulation tissue area was dramatically increased in the PLA group, and the time needed to achieve complete closure was 55% less in these patients compared to those in the collagen dressing group (9.8 ± 3.1 vs. 17.8 ± 11.2 weeks, p < 0.001). No complications were recorded during the trial.
Discussion: PLA matrices are more effective than active collagen dressings in promoting diabetic foot ulcer closure. Proposed reasons for this include controlled pore sizes that promote cell attachment, migration, and vascularization of the scaffolds; changes toward a neutral wound pH that may inhibit bacterial growth and promote cellular recruitment; and improved cellular signalling to promote neo-vascularization of the wound. This strategy can safely and effectively be used to promote wound closure and prevent limb amputation.
Methods: Patients with diabetes mellitus and a single foot ulcer of at least 3 months of evolution were randomized to receive either the weekly applications of a PLA matrix or collagen dressings as adjuncts to the standard of care. The wound size, the percentage of granulation tissue area, the number of weeks required to attain full closure, and the presence of complications, including infection, amputation, or treatment failure, were recorded. All patients were enrolled in a single high-volume center and were treated by the same surgeon. Analysis of the data was performed blindly by an independent researcher.
Results: A total of 28 patients were enrolled in the study (16 received PLA matrices and 12 collagen dressings). At baseline, the Hb1c, ABI, wound age, the percentage area of granulation tissue, and wound size was similar between the patient groups. All patients were followed until wound closure was attained. Granulation tissue area was dramatically increased in the PLA group, and the time needed to achieve complete closure was 55% less in these patients compared to those in the collagen dressing group (9.8 ± 3.1 vs. 17.8 ± 11.2 weeks, p < 0.001). No complications were recorded during the trial.
Discussion: PLA matrices are more effective than active collagen dressings in promoting diabetic foot ulcer closure. Proposed reasons for this include controlled pore sizes that promote cell attachment, migration, and vascularization of the scaffolds; changes toward a neutral wound pH that may inhibit bacterial growth and promote cellular recruitment; and improved cellular signalling to promote neo-vascularization of the wound. This strategy can safely and effectively be used to promote wound closure and prevent limb amputation.

.png)