Laboratory Research
(LR-009) Preliminary Evidence on the Barrier Properties of a PHMB-Impregnated Acellular Biologic Grafts for Treatment of Third-Degree Burns.
Friday, April 28, 2023
7:15 PM - 8:30 PM East Coast USA Time
Joel Gil, BS – Sr. Manager, Research Laboratory, Dr. Phillip Frost Department of Dermatology and Cutaneous Surgery, University of Miami Miller School of Medicine; Alexander Higa, MA – Research Associate 2, Dr. Phillip Frost Department of Dermatology and Cutaneous Surgery, University of Miami Miller School of Medicine; Michael Solis, MBA – Research Associate 2, Dr. Phillip Frost Department of Dermatology and Cutaneous Surgery, University of Miami Miller School of Medicine; Emily Buck, PhD – R&D Scientist, BioAesthetics Corporation; William Heim, MS, MBA, CTBS – Chief Operating Officer, BioAesthetics Corporation; Nicholas Pashos, PhD, CTBS – Chief Executive Officer, BioAesthetics Corporation
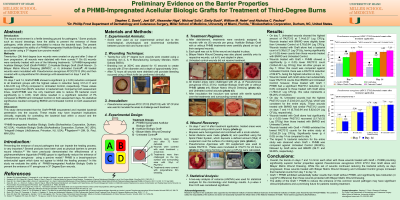
Introduction: The wound environment is a fertile breeding ground for pathogens.1 Some products such as wound dressings, have the ability to prevent the entrance of these pathogens, while others are formulated to reduce the bacterial load. The present study investigated the ability of a PHMB-Impregnated Acellular Biologic Grafts to act as a barrier using a 3rd degree burn porcine model.2
Methods: Twenty-four (24) third degree burn wounds were created on pig and after 3 days of burn progression, all wounds were debrided with 4mm currete.3,4 Six (6) wounds were randomly treated with one of the following treatments: 1) PHMB-Impregnated Acellular Biologic Graft (Graft+PHMB)^, 2) Acellular Biologic Graft (Graft Alone)+, 3) Bilayer Matrix Wound Dressing (BMWD)*, or 4) Untreated Control. All treated wounds were inoculated with Pseudomonas aeruginosa ATCC27312 (PA) and then covered with a polyurethane film dressings until assessment on days 7 and 14.
Results: On days 7 and 14, Graft+PHMB showed a significant (p ≤ 0.05) reduction compared to all treatments groups with the highest values in reduction being 3.51±0.11 and 4.60±0.05 Log CFU/g compared to untreated control, respectively. These values represent more than 99.9% reduction in bacterial load. Comparing both assessment times, Graft+PHMB was the only treatment able to reduce PA bacterial count significantly (p ≤ 0.05). Graft Alone resulted in a significant reduction of PA compared to BMWD and Untreated Control on both assessment days. No statistical significance resulted comparing BMWD and Untreated Control on both assessment days.
Discussion: This study demonstrated that the Graft+PHMB sequestered and impeded bacterial penetration into the wounds. These results may have important implications clinically, especially for controlling the bacterial load within a wound and the prevention of wound infections.
Methods: Twenty-four (24) third degree burn wounds were created on pig and after 3 days of burn progression, all wounds were debrided with 4mm currete.3,4 Six (6) wounds were randomly treated with one of the following treatments: 1) PHMB-Impregnated Acellular Biologic Graft (Graft+PHMB)^, 2) Acellular Biologic Graft (Graft Alone)+, 3) Bilayer Matrix Wound Dressing (BMWD)*, or 4) Untreated Control. All treated wounds were inoculated with Pseudomonas aeruginosa ATCC27312 (PA) and then covered with a polyurethane film dressings until assessment on days 7 and 14.
Results: On days 7 and 14, Graft+PHMB showed a significant (p ≤ 0.05) reduction compared to all treatments groups with the highest values in reduction being 3.51±0.11 and 4.60±0.05 Log CFU/g compared to untreated control, respectively. These values represent more than 99.9% reduction in bacterial load. Comparing both assessment times, Graft+PHMB was the only treatment able to reduce PA bacterial count significantly (p ≤ 0.05). Graft Alone resulted in a significant reduction of PA compared to BMWD and Untreated Control on both assessment days. No statistical significance resulted comparing BMWD and Untreated Control on both assessment days.
Discussion: This study demonstrated that the Graft+PHMB sequestered and impeded bacterial penetration into the wounds. These results may have important implications clinically, especially for controlling the bacterial load within a wound and the prevention of wound infections.

.png)