Laboratory Research
(LR-010) Effects of a Novel Non-Biologic Desiccant to Remove Bacteria Using a Deep Dermal Wound Porcine Model.
Friday, April 28, 2023
7:15 PM - 8:30 PM East Coast USA Time
Jie Li, MD, PhD – Associate Professor, Dr. Phillip Frost Department of Dermatology and Cutaneous Surgery, University of Miami, Miller School of Medicine. Dr. Phillip Frost Department of Dermatology and Cutaneous Surgery; Tongyu Wikramanayake, PhD – Associate Professor, Dr. Phillip Frost Department of Dermatology and Cutaneous Surgery, University of Miami, Miller School of Medicine. Dr. Phillip Frost Department of Dermatology and Cutaneous Surgery; Joel Gil, BS – Sr. Manager, Research Laboratory, Dr. Phillip Frost Department of Dermatology and Cutaneous Surgery, University of Miami, Miller School of Medicine. Dr. Phillip Frost Department of Dermatology and Cutaneous Surgery; Alexander Higa, MA – Research Associate 2, Dr. Phillip Frost Department of Dermatology and Cutaneous Surgery, University of Miami, Miller School of Medicine. Dr. Phillip Frost Department of Dermatology and Cutaneous Surgery; Michael Solis, MBA – Research Associate 2, Dr. Phillip Frost Department of Dermatology and Cutaneous Surgery, University of Miami, Miller School of Medicine. Dr. Phillip Frost Department of Dermatology and Cutaneous Surgery; Steven Kavros, DPM, MAPWCA, FACCWS – CHIEF MEDICAL OFFICER, EPIEN Medical, Inc
Introduction: Nosocomial infections are common in many healthcare provider and debridement plays a critical role in wound bed management. Debridement can eliminate necrotic tissue and bacteria that are harbored within the tissue.1 Infected wounds with drug-resistant bacteria (Staphylococcus aureus and Pseudomonas aeruginosa) have a high-risk of impending the healing process. Novel debridement method (novel molecular technology) was used in this study to remove necrotic tissue and bacteria from infected wounds using a porcine model.2,3
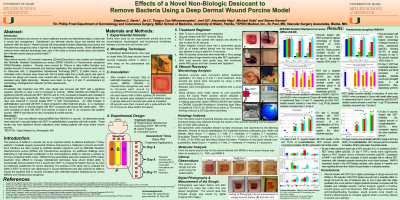
Methods: Deep dermal wounds (120wounds) measuring (22mmx22mmx3mm) were created and inoculated with Methicillin Resistant Staphylococcus aureus (MRSA USA300) or Pseudomonas aeruginosa PA09-010(military isolation). Wounds were covered for 72hours to allow biofilm formation and baseline wounds (3) were assessed prior treatment application, then remaining wounds were treated for 30seconds with: 1) Regenerative Debridement Technology[RDT*], 2) Gauze with sterile saline, or 3) Untreated control. Wounds were rinsed with 10ml of sterile saline then a sterile gauze was used to remove the slough and wounds were covered with a polyurethane film. Amount of slough was assessed using digital planimetry. Biopsies were taken on days 4, 8 and 11 post-treatment for microbiology, histological and molecular (rt-PCR) assessments.
Results: Immediately after treatment over 85% more slough was removed with RDT* with a significant reduction (p≤0.05) on days 4 and 8 compared to controls. MRSA USA300 and PA09-010 was significant (p≤0.05) reduced with RDT* (99.70% and 81.14%) compared to baseline and untreated in all assessment days, respectively. More than 1 LogCFU/g bacterial reduction compared day 11 to day4 was observed in wounds treated RDT* in both microorganisms. An initial increase in epithelialization was noted with RDT on day4 compared to other treatment groups. IL-1a expression was reduced (62%) in wounds treated with RDT* compared with Gauze with sterile saline. TNFa were increased on day4 with RDT* and reduced on Days 8 and 11, as compared with baseline wounds. MMP-9 was reduced on day 4 compared to control wounds.
Discussion: Overall, RDT* was most effective reducing MRSA than PA09-010 in wounds. No detrimental results were observeded in wounds treated with RDT* in epithelialization comparing with both controls. These results may have significant clinical implications when treating patients with acute and/or chronic wounds.
Methods: Deep dermal wounds (120wounds) measuring (22mmx22mmx3mm) were created and inoculated with Methicillin Resistant Staphylococcus aureus (MRSA USA300) or Pseudomonas aeruginosa PA09-010(military isolation). Wounds were covered for 72hours to allow biofilm formation and baseline wounds (3) were assessed prior treatment application, then remaining wounds were treated for 30seconds with: 1) Regenerative Debridement Technology[RDT*], 2) Gauze with sterile saline, or 3) Untreated control. Wounds were rinsed with 10ml of sterile saline then a sterile gauze was used to remove the slough and wounds were covered with a polyurethane film. Amount of slough was assessed using digital planimetry. Biopsies were taken on days 4, 8 and 11 post-treatment for microbiology, histological and molecular (rt-PCR) assessments.
Results: Immediately after treatment over 85% more slough was removed with RDT* with a significant reduction (p≤0.05) on days 4 and 8 compared to controls. MRSA USA300 and PA09-010 was significant (p≤0.05) reduced with RDT* (99.70% and 81.14%) compared to baseline and untreated in all assessment days, respectively. More than 1 LogCFU/g bacterial reduction compared day 11 to day4 was observed in wounds treated RDT* in both microorganisms. An initial increase in epithelialization was noted with RDT on day4 compared to other treatment groups. IL-1a expression was reduced (62%) in wounds treated with RDT* compared with Gauze with sterile saline. TNFa were increased on day4 with RDT* and reduced on Days 8 and 11, as compared with baseline wounds. MMP-9 was reduced on day 4 compared to control wounds.
Discussion: Overall, RDT* was most effective reducing MRSA than PA09-010 in wounds. No detrimental results were observeded in wounds treated with RDT* in epithelialization comparing with both controls. These results may have significant clinical implications when treating patients with acute and/or chronic wounds.

.png)