Laboratory Research
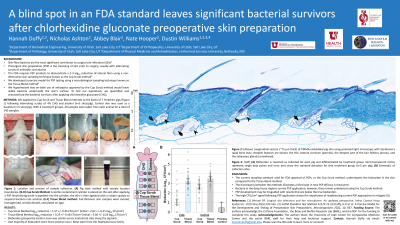
(LR-012(GR-007)) A blind spot in an FDA standard leaves significant bacterial survivors after chlorhexidine gluconate preoperative skin preparation
Friday, April 28, 2023
2:15 PM - 3:15 PM East Coast USA Time
Nic Ashton, PhD – Department of Orthopaedics – University of Utah; Nate Hooper, NA – Department of Orthopaedics – University of Utah; Abbey Blair, NA – Department of Orthopaedics – University of Utah; Dustin Williams, PhD – Department of Orthopaedics – University of Utah
Introduction:
Opportunistic pathogens of skin-flora origin constitute the most significant contributor to surgical site infections (SSIs) despite the ubiquitous use of presurgical skin preparations (PSPs). PSP is the cleansing of the skin prior to surgery, usually with alternating scrubs of antiseptic and alcohol. The FDA requires PSP products to demonstrate a 2-3 log10 reduction of natural flora using a non-destructive skin sampling technique. This process, known as the cup scrub method, consists of placing a sterile containment cylinder on the skin after applying a PSP. Neutralizing broth is pipetted into the cylinder; the skin is then agitated with a rubber spatula to suspend bacteria into solution.1 We hypothesize that on-label use of antiseptics approved by this cup scrub method leave viable bacteria underneath the skin's surface. Previously, we developed a porcine model for PSP testing using a microbiological sampling technique known as the tissue blend method: full-thickness skin samples were excised, homogenized, serially diluted, and plated on agar.2 To test our hypothesis, we quantified the bacterial survivors after applying a chlorhexidine gluconate (CHG) PSP using the cup scrub and tissue blend methods.
Methods:
We applied the cup scrub and tissue blend methods to the backs of 7 Yorkshire pigs following alternating scrubs of 4% CHG and alcohol (n=5 sites/pig). Control skin was used as a baseline (n=5 sites/pig). With 4 treatment groups, 20 samples were taken from each animal for a total of 140 samples.
Results:
The average log10 reduction for the cup scrub and tissue blend methods were 1.57 +/- 0.45 CFU/cm2 and 0.23 +/- 0.48 CFU/cm2, respectively. Initial bioburden values using the cup scrub and tissue blend methods were 2.62 +/- 0.21 CFU/cm2 and 3.46 +/- 0.24 CFU/cm2, respectively. The difference in bioburden between the techniques was statistically significant (p < 0.001).
Discussion:
Most SSIs stem from skin flora bacteria.3 This dangerous and costly complication is principally prevented by PSP application. The current sampling standard used for FDA approval of PSPs, or the cup scrub method, underreports the bioburden in the skin compared to the tissue blend method. This discrepancy illustrates a blind spot in how PSP efficacy is measured. Bacteria in the deep tissue regions survive PSP application; however, they remain undetected. Thus, PSP development may be misguided with results that are below the true bioburden. The high CFU/cm2 signal following PSP application with the tissue blend method shows the importance of readdressing current PSP approaches to mitigating SSI.
Opportunistic pathogens of skin-flora origin constitute the most significant contributor to surgical site infections (SSIs) despite the ubiquitous use of presurgical skin preparations (PSPs). PSP is the cleansing of the skin prior to surgery, usually with alternating scrubs of antiseptic and alcohol. The FDA requires PSP products to demonstrate a 2-3 log10 reduction of natural flora using a non-destructive skin sampling technique. This process, known as the cup scrub method, consists of placing a sterile containment cylinder on the skin after applying a PSP. Neutralizing broth is pipetted into the cylinder; the skin is then agitated with a rubber spatula to suspend bacteria into solution.1 We hypothesize that on-label use of antiseptics approved by this cup scrub method leave viable bacteria underneath the skin's surface. Previously, we developed a porcine model for PSP testing using a microbiological sampling technique known as the tissue blend method: full-thickness skin samples were excised, homogenized, serially diluted, and plated on agar.2 To test our hypothesis, we quantified the bacterial survivors after applying a chlorhexidine gluconate (CHG) PSP using the cup scrub and tissue blend methods.
Methods:
We applied the cup scrub and tissue blend methods to the backs of 7 Yorkshire pigs following alternating scrubs of 4% CHG and alcohol (n=5 sites/pig). Control skin was used as a baseline (n=5 sites/pig). With 4 treatment groups, 20 samples were taken from each animal for a total of 140 samples.
Results:
The average log10 reduction for the cup scrub and tissue blend methods were 1.57 +/- 0.45 CFU/cm2 and 0.23 +/- 0.48 CFU/cm2, respectively. Initial bioburden values using the cup scrub and tissue blend methods were 2.62 +/- 0.21 CFU/cm2 and 3.46 +/- 0.24 CFU/cm2, respectively. The difference in bioburden between the techniques was statistically significant (p < 0.001).
Discussion:
Most SSIs stem from skin flora bacteria.3 This dangerous and costly complication is principally prevented by PSP application. The current sampling standard used for FDA approval of PSPs, or the cup scrub method, underreports the bioburden in the skin compared to the tissue blend method. This discrepancy illustrates a blind spot in how PSP efficacy is measured. Bacteria in the deep tissue regions survive PSP application; however, they remain undetected. Thus, PSP development may be misguided with results that are below the true bioburden. The high CFU/cm2 signal following PSP application with the tissue blend method shows the importance of readdressing current PSP approaches to mitigating SSI.

.png)