Laboratory Research
(LR-014) Effects of a Novel Non-Biologic Desiccant to Remove Dermatophytes Using a Deep Partial Thickness Wound Porcine Model.
Friday, April 28, 2023
7:15 PM - 8:30 PM East Coast USA Time
Alexander Higa, MA – Research Associate 2, Dr. Phillip Frost Department of Dermatology and Cutaneous Surgery, University of Miami, Miller School of Medicine. Dr. Phillip Frost Department of Dermatology and Cutaneous Surgery; Michael Solis, MBA – Research Associate 2, Dr. Phillip Frost Department of Dermatology and Cutaneous Surgery, University of Miami, Miller School of Medicine. Dr. Phillip Frost Department of Dermatology and Cutaneous Surgery; Steven Kavros, DPM, MAPWCA, FACCWS – CHIEF MEDICAL OFFICER, EPIEN Medical, Inc; Stephen Davis, BS – Research Professor, Dr. Phillip Frost Department of Dermatology and Cutaneous Surgery, University of Miami, Miller School of Medicine. Dr. Phillip Frost Department of Dermatology and Cutaneous Surgery
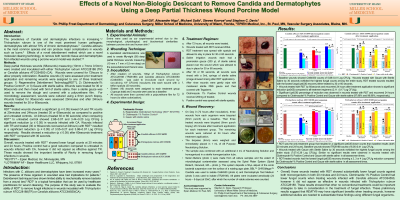
Introduction: The prevalence of Candida and dermatophye infections is increasing.1,2 Trichophyton rubrum is one of the most prominant human pathogenic dermatophytes with almost 70% of chronic dermatophytoses.2 Candida albicans is the most common species and can produce major complicantions in wounds such as burns.3. Effects of a novel debridement method which use a novel molecular cleaning technology, to remove both necrotic tissue and dermatophytes from infected wounds using a porcine wound model was studied. 4,5
Methods: Deep partial thickness wounds (58wounds) measuring (10mm x 7mmx 0.5mm) were created and inoculated with either Trichophyton rubrum ATCC28188 (TR) or Candida albicans ATCC64550 (CA). Wounds were covered for 72hours to allow properly colonization. Baseline wounds (3) were assessed prior treatment application and remaining wounds were assigned to one of three treatment groups: 1) Regenerative Debridement Technology[RDT*], 2) Clotrimazole1% Positive ControlÉ, or 3) Gauze with sterile saline. Wounds were treated for 30 or 60seconds and then rinsed with 5ml of sterile saline, then a sterile gauze was used to remove the slough and covered with a polyurethane film. For microbiology assessment, wounds were cultured using a 6mm punch biopsy. Wounds treated for 30seconds were assessed 20minutes and after 24hours wounds treated for 30 or 60seconds.
Results: RDT* treated wounds showed a significant (p ≤ 0.05) lowest CA and TR counts at 20minutes and 24hours (treated 30 or 60seconds) as compared to positive and untreated controls. At 24hours (treated 30 or 60 seconds) when comparing RDT* to untreated control showed 2.68±0.07 and 3.44±0.20 Log CFU/g a significant reduction (p ≤ 0.05) in wounds infected with CA. Wounds infected with TR and treated (30 or 60seconds recovered at 24hours) with RDT* resulted in a significant reduction (p ≤ 0.05) of 3.55±0.27 and 3.98±0.07 Log CFU/g respectively. Results showed a reduction (p ≤ 0.05) after 60seconds treatment with RDT* compared with 30 seconds.
Discussion: Overall, wounds treated with RDT* showed lower fungal counts at 20 minutes and 24 hours. Positive control had a good reduction compared to untreated in wounds infected with CA, however it did not appear as effective against TR. These results showed the important benefits of Revity in removing fungal infections in wounds.
Methods: Deep partial thickness wounds (58wounds) measuring (10mm x 7mmx 0.5mm) were created and inoculated with either Trichophyton rubrum ATCC28188 (TR) or Candida albicans ATCC64550 (CA). Wounds were covered for 72hours to allow properly colonization. Baseline wounds (3) were assessed prior treatment application and remaining wounds were assigned to one of three treatment groups: 1) Regenerative Debridement Technology[RDT*], 2) Clotrimazole1% Positive ControlÉ, or 3) Gauze with sterile saline. Wounds were treated for 30 or 60seconds and then rinsed with 5ml of sterile saline, then a sterile gauze was used to remove the slough and covered with a polyurethane film. For microbiology assessment, wounds were cultured using a 6mm punch biopsy. Wounds treated for 30seconds were assessed 20minutes and after 24hours wounds treated for 30 or 60seconds.
Results: RDT* treated wounds showed a significant (p ≤ 0.05) lowest CA and TR counts at 20minutes and 24hours (treated 30 or 60seconds) as compared to positive and untreated controls. At 24hours (treated 30 or 60 seconds) when comparing RDT* to untreated control showed 2.68±0.07 and 3.44±0.20 Log CFU/g a significant reduction (p ≤ 0.05) in wounds infected with CA. Wounds infected with TR and treated (30 or 60seconds recovered at 24hours) with RDT* resulted in a significant reduction (p ≤ 0.05) of 3.55±0.27 and 3.98±0.07 Log CFU/g respectively. Results showed a reduction (p ≤ 0.05) after 60seconds treatment with RDT* compared with 30 seconds.
Discussion: Overall, wounds treated with RDT* showed lower fungal counts at 20 minutes and 24 hours. Positive control had a good reduction compared to untreated in wounds infected with CA, however it did not appear as effective against TR. These results showed the important benefits of Revity in removing fungal infections in wounds.

.png)