Laboratory Research
(LR-026) Photodynamic Therapy Effects in Skin of Color Wound Healing: an In Vitro Investigation
Friday, April 28, 2023
7:15 PM - 8:30 PM East Coast USA Time
Felix Fang, B.S. – Medical Student, School of Medicine, University of Texas Medical Branch; Michael Wilkerson, M.D. – Professor and Chair, Dermatology, University of Texas Medical Branch; Amina El Ayadi, PhD – Assistant Professor, Surgery, University of Texas Medical Branch
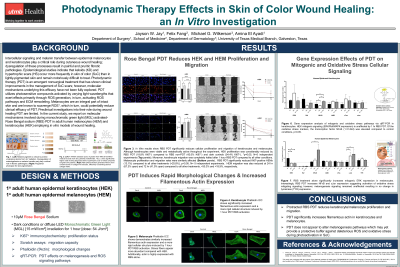
Introduction: Epidemiological studies indicate that keloids (KD) and hypertrophic scars (HS) occur more frequently in skin of color (SoC) than in lightly-pigmented skin and remain notoriously difficult to treat. Photodynamic therapy (PDT) is an emergent nonsurgical treatment that has shown clinical improvements in the management of SoC scars; however, molecular mechanisms underlying this efficacy have not been explored. PDT utilizes photosensitive compounds activated by varying light wavelengths that exert effects primarily through ROS generation, in turn, activating ROS pathways and ECM remodeling. Melanocytes are an integral part of intact skin and are known to scavenge ROS, but investigations into their role during wound healing PDT are limited. In the current study, we report on molecular mechanisms involved during monochromatic green light (MGL) activated-Rose Bengal sodium (RBS) PDT in adult human melanocytes (HEM) and keratinocytes (HEK) employing in vitro models of wound healing.
Methods: HEM and HEK were treated with 10μM RBS with and without 1-hour photoactivation in normal culture conditions. Cellular morphology, proliferation, and migration were assessed through immunocytochemistry and scratch assays. Specific gene targets involved in melanogenesis and redox signaling were assessed through RT-qPCR.
Results: RBS-PDT significantly reduced keratinocyte and melanocyte proliferation and migration compared non-PDT controls (p< 0.05). Both HEK and HEM morphology were significantly altered with RBS-PDT and expressed a more rigid cellular structure with increased presence of filamentous actin. NFκB gene expression was significantly elevated in HEK and HEM treated with RBS-PDT, while ERK expression was markedly decreased in HEM. Additionally, cJun transcripts were also significantly elevated with RBS-PDT in HEM (p< 0.05). Moreover, tyrosinase expression remained unchanged for HEM in all treatments.
Discussion: Taken together, these data suggest that protracted RBS-PDT has the capacity to diminish both keratinocyte and melanocyte proliferation and migration through modulation of transcription factors important in ROS-mitigating signaling, cell survival, and increased cytoskeletal rigidity. Importantly, RBS-PDT did not alter melanogenesis and may provide a protective buffer against deleterious ROS during photoactivation. Collectively, this pilot data demonstrates that PDT may offer a useful adjuvant with emergent therapies to improve cutaneous wound healing in anti-fibrotic treatments for SoC.
Methods: HEM and HEK were treated with 10μM RBS with and without 1-hour photoactivation in normal culture conditions. Cellular morphology, proliferation, and migration were assessed through immunocytochemistry and scratch assays. Specific gene targets involved in melanogenesis and redox signaling were assessed through RT-qPCR.
Results: RBS-PDT significantly reduced keratinocyte and melanocyte proliferation and migration compared non-PDT controls (p< 0.05). Both HEK and HEM morphology were significantly altered with RBS-PDT and expressed a more rigid cellular structure with increased presence of filamentous actin. NFκB gene expression was significantly elevated in HEK and HEM treated with RBS-PDT, while ERK expression was markedly decreased in HEM. Additionally, cJun transcripts were also significantly elevated with RBS-PDT in HEM (p< 0.05). Moreover, tyrosinase expression remained unchanged for HEM in all treatments.
Discussion: Taken together, these data suggest that protracted RBS-PDT has the capacity to diminish both keratinocyte and melanocyte proliferation and migration through modulation of transcription factors important in ROS-mitigating signaling, cell survival, and increased cytoskeletal rigidity. Importantly, RBS-PDT did not alter melanogenesis and may provide a protective buffer against deleterious ROS during photoactivation. Collectively, this pilot data demonstrates that PDT may offer a useful adjuvant with emergent therapies to improve cutaneous wound healing in anti-fibrotic treatments for SoC.

.png)