Laboratory Research
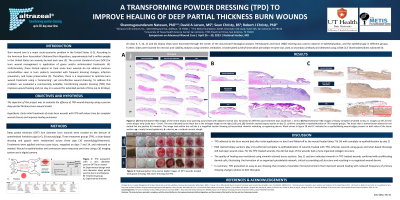
(LR-038) A Transforming Powder Dressing (TPD*) to Improve Healing of Deep Partial Thickness Burn Wounds
Friday, April 28, 2023
7:15 PM - 8:30 PM East Coast USA Time
Robert Christy, PhD – Deputy Director, Military Health Institute, University of Texas Health Science Center; Sean Christy, BS – Biomedical Research Assistant, The Metis Foundation; David Larson, MS – Biomedical Research Associate, The Metis Foundation
Introduction: According to the American Burn Association’s National Burn Repository, approximately half a million people in the United States are severely burned each year. The current standard of care for burn wound management is application of gauze and/or antimicrobial treatments. Unfortunately, these limited options to treat acute burn wounds do not address common comorbidities seen in burn patients including pain associated with frequent dressing changes, infection prevention, and tissue preservation. We used a porcine deep partial thickness burn wound model to evaluate a novel, commercially available, transforming powder dressing (TPD) that improves wound healing and can stay on a wound for extended periods of time (up to 30 days).
Methods: Deep partial thickness burn wounds with 3 cm diameter were created on the dorsum of anesthetized Yorkshire pigs (30 wounds/pig, n=3). Three treatment groups, randomized across three pigs (TPD, a silver-based dressing and gauze; 10wounds/pig/treatment) were applied 1-hour post-injury and on days 7 and 14 or in between as needed. Wound re-epithelization and contraction were measured over time using a 3D imaging system and a digital camera. On days 0, 7, 14, 21 and 28, biopsy strips were harvested through the center of the wound bed and subjected to histological analysis to document wound healing.
Results: Results indicated that TPD adhered to the burn wound bed after initial application on day 0 and flaked-off as the wound healed (days 7 and 14) with complete re-epithelialization by day 28. Histological analysis of day 28 biopsy sections confirmed complete re-epithelialization of wounds treated with TPD, whereas wounds using gauze and silver-based dressing still had open wound areas. For the TPD treated wounds, the dermal layer of the wounds had a more organized collagen structure and less inflammatory cell infiltration in comparison to the control wounds.
Discussion: TPD is an easy-to-use dressing that reduces the frequency of dressing changes required for acute deep partial thickness burn treatment and creates a favorable microenvironment that improves wound healing.
Applicability of Research to Practice: TPD provides an ideal dressing option for use in both immediate coverages, as well as long-term burn wound care management.
Methods: Deep partial thickness burn wounds with 3 cm diameter were created on the dorsum of anesthetized Yorkshire pigs (30 wounds/pig, n=3). Three treatment groups, randomized across three pigs (TPD, a silver-based dressing and gauze; 10wounds/pig/treatment) were applied 1-hour post-injury and on days 7 and 14 or in between as needed. Wound re-epithelization and contraction were measured over time using a 3D imaging system and a digital camera. On days 0, 7, 14, 21 and 28, biopsy strips were harvested through the center of the wound bed and subjected to histological analysis to document wound healing.
Results: Results indicated that TPD adhered to the burn wound bed after initial application on day 0 and flaked-off as the wound healed (days 7 and 14) with complete re-epithelialization by day 28. Histological analysis of day 28 biopsy sections confirmed complete re-epithelialization of wounds treated with TPD, whereas wounds using gauze and silver-based dressing still had open wound areas. For the TPD treated wounds, the dermal layer of the wounds had a more organized collagen structure and less inflammatory cell infiltration in comparison to the control wounds.
Discussion: TPD is an easy-to-use dressing that reduces the frequency of dressing changes required for acute deep partial thickness burn treatment and creates a favorable microenvironment that improves wound healing.
Applicability of Research to Practice: TPD provides an ideal dressing option for use in both immediate coverages, as well as long-term burn wound care management.

.png)