Laboratory Research
(LR-050) The Antimicrobial and Wound Healing Effects of a Novel Hydrogel Combat Gauze with Copper on Third-Degree Burns Using a Porcine Model.
Friday, April 28, 2023
7:15 PM - 8:30 PM East Coast USA Time
Jie Li, MD, PhD – Associate Professor, Dr. Phillip Frost Department of Dermatology and Cutaneous Surgery, University of Miami, Miller School of Medicine. Dr. Phillip Frost Department of Dermatology and Cutaneous Surgery; Joel Gil, BS – Sr. Manager, Research Laboratory, Dr. Phillip Frost Department of Dermatology and Cutaneous Surgery, University of Miami, Miller School of Medicine. Dr. Phillip Frost Department of Dermatology and Cutaneous Surgery; Alexander Higa, MA – Research Associate 2, Dr. Phillip Frost Department of Dermatology and Cutaneous Surgery, University of Miami, Miller School of Medicine. Dr. Phillip Frost Department of Dermatology and Cutaneous Surgery; Aaron Strickland, PhD – Vice President of Research and Development, iFyber, LLC; Stephen Davis, BS – Research Professor, Dr. Phillip Frost Department of Dermatology and Cutaneous Surgery, University of Miami, Miller School of Medicine. Dr. Phillip Frost Department of Dermatology and Cutaneous Surgery
Introduction: Methicillin-resistant Staphylococcus aureus (MRSA) is one of the most commonly encountered bacteria in the burn unit and can be challenging to iradicate.1 Copper has been previously shown to have antimicrobial activity against various pathogens.2 There has also been reported wound healing effects with the use of copper.3 The present study was performed to investigate the antimicrobial and wound healing activity of two novel hydrogel formulations with coppper and their ability to enhance the healing using a 3rd degree burn porcine model.4
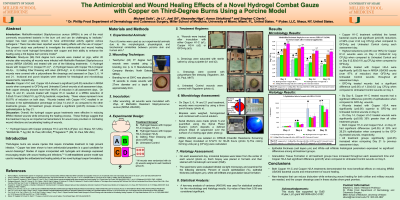
Methods: Ninety-six (96) third degree burn wounds were created on pig, within 20 minutes after wounding all wounds were infected with Methicillin Resistant Staphylococcus aureus (MRSA USA300) and treated with one of the following treatments: 1) Hydrogel Gauze with Copper H1-C (Copper H1-C)^, 2) Hydrogel Gauze with Copper H2-A (Copper H2-A)+, 3) Gelling Fiber Dressing with silver (GFD-Ag)*, or 4) Untreated Control. All wounds were covered with a polyurethane film dressings and assesseed on days 3, 6, 14 and 21. Incisional and punch biopsies were obtained for histological and microbiologogy assessments, respectively.
Results: Copper H1-C and Copper H2-A showed a significant (p≤0.05) reduction in MRSA counts when compared to GFD-Ag and untreated control wounds at all assessment days. Both copper dressing showed more than 99.8% of reduction in all assessment days. On days 14 and 21, wounds treated with Copper H1-C resulted in a MRSA reduction of 3.55±0.10 and 3.58±0.10 Log CFU/g bacterial, respectively. These values represent more 99.97% of reduction in both days. Wounds treated with Copper H1-C resulted in a increase in the epithelialization percentage on days 14 and 21 as compared to the other treatments groups. All treatment groups showed a significant (p≤0.05) increase in the ephitelializaytion by day 21.
Discussion: Overall, the hydrogel copper gauze treatments were effective in reducing MRSA infected wounds while enhancing the healing process. These findings suggest that this treatment may be an important armamentarium for wound care providers in combating wound infections and acceralting healing of wounds.
Methods: Ninety-six (96) third degree burn wounds were created on pig, within 20 minutes after wounding all wounds were infected with Methicillin Resistant Staphylococcus aureus (MRSA USA300) and treated with one of the following treatments: 1) Hydrogel Gauze with Copper H1-C (Copper H1-C)^, 2) Hydrogel Gauze with Copper H2-A (Copper H2-A)+, 3) Gelling Fiber Dressing with silver (GFD-Ag)*, or 4) Untreated Control. All wounds were covered with a polyurethane film dressings and assesseed on days 3, 6, 14 and 21. Incisional and punch biopsies were obtained for histological and microbiologogy assessments, respectively.
Results: Copper H1-C and Copper H2-A showed a significant (p≤0.05) reduction in MRSA counts when compared to GFD-Ag and untreated control wounds at all assessment days. Both copper dressing showed more than 99.8% of reduction in all assessment days. On days 14 and 21, wounds treated with Copper H1-C resulted in a MRSA reduction of 3.55±0.10 and 3.58±0.10 Log CFU/g bacterial, respectively. These values represent more 99.97% of reduction in both days. Wounds treated with Copper H1-C resulted in a increase in the epithelialization percentage on days 14 and 21 as compared to the other treatments groups. All treatment groups showed a significant (p≤0.05) increase in the ephitelializaytion by day 21.
Discussion: Overall, the hydrogel copper gauze treatments were effective in reducing MRSA infected wounds while enhancing the healing process. These findings suggest that this treatment may be an important armamentarium for wound care providers in combating wound infections and acceralting healing of wounds.

.png)
