Clinical Research
(DLS-034) Chronological impact of social determinants of health affecting patient adherence to chronic wound follow-up after discharge
Friday, April 28, 2023
7:15 PM - 8:30 PM East Coast USA Time
Adrian Chen, B.S. – Visiting Scholar, Biomedical Sciences Lab, Northwell Health; Amit Rao, M.D. – Project Manager, Surgery, Northwell Health
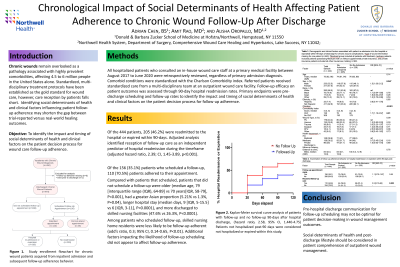
Introduction: Chronic wounds remain overlooked as a pathology associated with highly prevalent comorbidities, affecting 4.5 to 6 million people in the United States alone. Standardized, multi-disciplinary treatment protocols have been established as the gold standard for wound care, however, care reception by patients falls short. Identifying social determinants of health and clinical factors influencing patient follow-up adherence may shorten the gap between trial-reported versus real-world healing outcomes. This study's objective was to identify the impact and timing of social determinants of health and clinical factors on the patient decision process for wound care follow-up adherence.
Methods: All hospitalized patients who consulted an in-house wound care staff at a primary medical facility between August 2017 to June 2020 were retrospectively reviewed, regardless of primary admission diagnosis. Comorbid conditions were standardized with the Charlson Comorbidity index. Referred patients received standardized care from a multi-disciplinary team at an outpatient wound care facility. Follow-up efficacy on patient outcomes was assessed through 90-day hospital readmission rates. Primary endpoints were pre-discharge scheduling and follow-up rates to identify the impact and timing of social determinants of health and clinical factors on the patient decision process for follow-up adherence.
Results: Of the 444 patients, 205 (46.2%) were readmitted to the hospital or expired within 90-days. Adjusted analysis identified reception of follow-up care as an independent predictor of hospital readmission during the timeframe (adjusted hazard ratio, 2.39; 95% CI, 1.45-3.89, p< 0.001). Of the 156 (35.1%) patients who scheduled a follow-up, 110 (70.5%) patients adhered to their appointment. Compared with patients that scheduled, patients that did not schedule a follow-up were older (median age, 79 [interquartile range (IQR), 64-89] vs 70 years [IQR, 58-79], P< 0.001), had a greater Asian proportion (5.21% vs 1.3%, P=0.04), longer hospital stay (median days, 9 [IQR, 5-15.5] vs 6 [IQR, 3-11], P< 0.0001), and more discharged to skilled nursing facilities (47.6% vs 26.3%, P< 0.0001). Among patients who scheduled follow-up, skilled nursing home residents were less likely to be follow-up adherent (odd’s ratio, 0.3; 95% CI, 0.14-0.65, P< 0.01). Additional factors impacting the likelihood of follow-up scheduling did not appear to affect follow-up adherence.
Discussion: Pre-hospital discharge communication for follow-up scheduling may not be optimal for patient decision-making in wound management outcomes. Social determinants of health and post-discharge lifestyle should be considered in patient comprehension of outpatient wound management.
Methods: All hospitalized patients who consulted an in-house wound care staff at a primary medical facility between August 2017 to June 2020 were retrospectively reviewed, regardless of primary admission diagnosis. Comorbid conditions were standardized with the Charlson Comorbidity index. Referred patients received standardized care from a multi-disciplinary team at an outpatient wound care facility. Follow-up efficacy on patient outcomes was assessed through 90-day hospital readmission rates. Primary endpoints were pre-discharge scheduling and follow-up rates to identify the impact and timing of social determinants of health and clinical factors on the patient decision process for follow-up adherence.
Results: Of the 444 patients, 205 (46.2%) were readmitted to the hospital or expired within 90-days. Adjusted analysis identified reception of follow-up care as an independent predictor of hospital readmission during the timeframe (adjusted hazard ratio, 2.39; 95% CI, 1.45-3.89, p< 0.001). Of the 156 (35.1%) patients who scheduled a follow-up, 110 (70.5%) patients adhered to their appointment. Compared with patients that scheduled, patients that did not schedule a follow-up were older (median age, 79 [interquartile range (IQR), 64-89] vs 70 years [IQR, 58-79], P< 0.001), had a greater Asian proportion (5.21% vs 1.3%, P=0.04), longer hospital stay (median days, 9 [IQR, 5-15.5] vs 6 [IQR, 3-11], P< 0.0001), and more discharged to skilled nursing facilities (47.6% vs 26.3%, P< 0.0001). Among patients who scheduled follow-up, skilled nursing home residents were less likely to be follow-up adherent (odd’s ratio, 0.3; 95% CI, 0.14-0.65, P< 0.01). Additional factors impacting the likelihood of follow-up scheduling did not appear to affect follow-up adherence.
Discussion: Pre-hospital discharge communication for follow-up scheduling may not be optimal for patient decision-making in wound management outcomes. Social determinants of health and post-discharge lifestyle should be considered in patient comprehension of outpatient wound management.

.png)
