Clinical Research
(CR-005) Multi-center, Randomized Controlled Clinical Investigation Evaluating a Unique Micro Water Jet Technology Device Versus Standard Debridement in the Treatment of Diabetic Foot.
Friday, April 28, 2023
7:15 PM - 8:30 PM East Coast USA Time
Robert Galiano, MD – Professor of Surgery, Northwestern University School of Medicine; Dennis Orgill, MD, PhD – Professor of Surgery, Harvard; Paul Glat, MD – Professor of Surgery, Drexel University; Marissa Carter, PhD – Strategic Solutions; Charles Zelen, DPM – Medical Director, Research, PERI
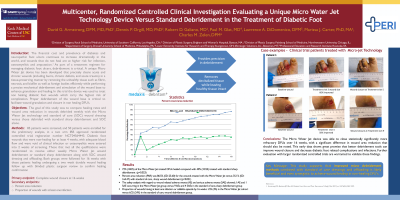
Introduction: A unique micro water jet device has been developed that precisely cleans acute and chronic wounds in a tissue-preserving manner by removing the unhealthy tissue such as fibrin, necrosis, and biofilm as well as foreign bodies efficiently while performing a precise mechanical cleaning and stimulation of the wound base to enhance granulation and healing. Proper debridement of the wound base is critical to facilitate wound granulation and closure in non healing DFU’s. The goal of this study was to compare healing rates and wound area reduction in wounds debrided weekly with the Micro Water Jet technology and standard of care(SOC)wound dressing versus those debrided with standard sharp debridement and SOC alone
Methods: 85 patients were screened, and 50 patients were enrolled for the preliminary analysis, in a two arm randomized controlled trial. Diabetic foot wounds that were non-healing for at least 4 weeks, with adequate blood flow and were void of clinical infection or osteomyelitis were entered into 2 weeks of screening. Those that met all the qualifications were randomized to receive either weekly micro jet wound debridement or standard sharp debridement along with SOC wound dressing and offloading. Both groups were followed for 16 weeks with those patients healing undergoing a two week durable wound healing follow up with blinded plastic surgeon review to confirm healing confirmation. The study endpoints included healing at 16 weeks as well as percent area wound reduction(PAR)over the treatment phase of 16 weeks.
Results: At 16 weeks 72%(18/25) of the Micro Water jet treated DFUs healed compared with 40%(10/25) treated with standard sharp debridement p=0.023(unadjusted). Furthermore, at 16 weeks, the percent area reduction(PAR) was 86.5%(SD: 25.60) for the wounds treated with the Micro Water Jet versus 35.1% (SD: 164.47) with standard sharp wound debridement p=0.021(unadjusted). The safety analysis showed with regard to wound related adverse events(AE) and serious adverse events(SAE); 1 AE and 1 SAE occurring in the Micro Water jet group versus 9 AEs and 4 SAEs in the standard sharp debridement group. Proportion of wounds having at least one infection or cellulitis episode by 16 weeks 1/25(4%) in the Micro Water Jet cohort versus 6/25(24%) in the standard wound debridement group
Discussion: The micro water jet device was able to statistically significantly close more refractory DFUs over 16 weeks, Therefore, early data shows great promise that better debridement tools can improve wound closure and decrease diabetic foot related complications and infections.
Methods: 85 patients were screened, and 50 patients were enrolled for the preliminary analysis, in a two arm randomized controlled trial. Diabetic foot wounds that were non-healing for at least 4 weeks, with adequate blood flow and were void of clinical infection or osteomyelitis were entered into 2 weeks of screening. Those that met all the qualifications were randomized to receive either weekly micro jet wound debridement or standard sharp debridement along with SOC wound dressing and offloading. Both groups were followed for 16 weeks with those patients healing undergoing a two week durable wound healing follow up with blinded plastic surgeon review to confirm healing confirmation. The study endpoints included healing at 16 weeks as well as percent area wound reduction(PAR)over the treatment phase of 16 weeks.
Results: At 16 weeks 72%(18/25) of the Micro Water jet treated DFUs healed compared with 40%(10/25) treated with standard sharp debridement p=0.023(unadjusted). Furthermore, at 16 weeks, the percent area reduction(PAR) was 86.5%(SD: 25.60) for the wounds treated with the Micro Water Jet versus 35.1% (SD: 164.47) with standard sharp wound debridement p=0.021(unadjusted). The safety analysis showed with regard to wound related adverse events(AE) and serious adverse events(SAE); 1 AE and 1 SAE occurring in the Micro Water jet group versus 9 AEs and 4 SAEs in the standard sharp debridement group. Proportion of wounds having at least one infection or cellulitis episode by 16 weeks 1/25(4%) in the Micro Water Jet cohort versus 6/25(24%) in the standard wound debridement group
Discussion: The micro water jet device was able to statistically significantly close more refractory DFUs over 16 weeks, Therefore, early data shows great promise that better debridement tools can improve wound closure and decrease diabetic foot related complications and infections.

.png)
