Clinical Research
(CR-015) Comparative Effectiveness Analyses for Medicare Beneficiaries with Diabetic Foot Ulcers Treated With and Without a Native Collagen Extracellular Matrix Plus Polyhexamethylene Biguanide (PHMB) Antimicrobial Barrier (PCMP)
Friday, April 28, 2023
7:15 PM - 8:30 PM East Coast USA Time
Justin Chun, MHS; Jian-Yu e, ScD; Robert Kirsner, MD, PhD; Serena Kongara, MPH; Braford Rice, PhD
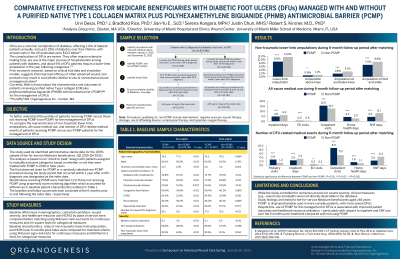
Introduction: Native collagen extracellular matrix plus PHMB antimicrobial barrier* (PCMP) is FDA-cleared for the management of acute and chronic wounds, including diabetic foot ulcers (DFUs). However, there is limited information about the real-world clinical and economic outcomes (i.e., healthcare resource utilization and costs) associated with using PCMP* for people with DFUs.
Methods: The 100% Medicare Fee-For-Service data in Standard Analytic File (Q1 2015-Q4 2021) were used to identify two mutually-exclusive cohorts of beneficiaries with DFUs: (i) beneficiaries who received PCMP* (first claim was considered the index date), and (ii) beneficiaries who received advanced wound care (e.g., debridement, offloading, negative pressure wound therapy) but not PCMP* (index date selected at random). Beneficiaries were required to have continuous enrollment in Medicare Parts A and B at least 6 months before and after the index date. Beneficiaries receiving PCMP* were matched 1:1 to those not receiving PCMP* using propensity score matching. Outcomes over 6 months post-index were compared between matched cohorts using statistical tests for paired data. Standardized differences (SD) >10% and p-values < 0.05 were considered statistically significant.
Results: Among all beneficiaries meeting the selection criteria, 12,679 received PCMP* and 578,781 did not receive PCMP*. Compared to beneficiaries not receiving PCMP*, those receving PCMP* had greater disease severity before treatment initiation as indicated by longer duration of active ulceration (6.2 vs. 3.6 months), higher rates of DFU-related infections (68.2% vs. 48.9%), non-traumatic lower-limb amputations (10.5% vs. 6.8%), and higher total medical costs ($36,108.3 vs. $23,915.9). During 6-month follow-up period, matched beneficiaries receiving PCMP* (N=12,587) had lower rates of non-traumatic lower-limb amputations (8.9% vs. 11.6%; SD = -9.13%; p < 0.001), as well as shorter stays and lower costs for hospitalization (4.8 vs. 6.2 days; $10,519.2 vs. $13,155.1) and skilled nursing facility (4.4 vs. 8.1 days; $1,968.1 vs. $3,210.6; SD >10% and p < 0.001 for all comparisons) than similar beneficiaries not receiving PCMP*.
Discussion: The study suggests that PCMP* is disproportionately used to treat more complex beneficiaries, with more severe DFUs. After adjusting for baseline differences, beneficiaries receiving PCMP* had lower rates of amputations, and lower costs for hospitalization and skilled nursing facility visits than those not receiving PCMP*.
Methods: The 100% Medicare Fee-For-Service data in Standard Analytic File (Q1 2015-Q4 2021) were used to identify two mutually-exclusive cohorts of beneficiaries with DFUs: (i) beneficiaries who received PCMP* (first claim was considered the index date), and (ii) beneficiaries who received advanced wound care (e.g., debridement, offloading, negative pressure wound therapy) but not PCMP* (index date selected at random). Beneficiaries were required to have continuous enrollment in Medicare Parts A and B at least 6 months before and after the index date. Beneficiaries receiving PCMP* were matched 1:1 to those not receiving PCMP* using propensity score matching. Outcomes over 6 months post-index were compared between matched cohorts using statistical tests for paired data. Standardized differences (SD) >10% and p-values < 0.05 were considered statistically significant.
Results: Among all beneficiaries meeting the selection criteria, 12,679 received PCMP* and 578,781 did not receive PCMP*. Compared to beneficiaries not receiving PCMP*, those receving PCMP* had greater disease severity before treatment initiation as indicated by longer duration of active ulceration (6.2 vs. 3.6 months), higher rates of DFU-related infections (68.2% vs. 48.9%), non-traumatic lower-limb amputations (10.5% vs. 6.8%), and higher total medical costs ($36,108.3 vs. $23,915.9). During 6-month follow-up period, matched beneficiaries receiving PCMP* (N=12,587) had lower rates of non-traumatic lower-limb amputations (8.9% vs. 11.6%; SD = -9.13%; p < 0.001), as well as shorter stays and lower costs for hospitalization (4.8 vs. 6.2 days; $10,519.2 vs. $13,155.1) and skilled nursing facility (4.4 vs. 8.1 days; $1,968.1 vs. $3,210.6; SD >10% and p < 0.001 for all comparisons) than similar beneficiaries not receiving PCMP*.
Discussion: The study suggests that PCMP* is disproportionately used to treat more complex beneficiaries, with more severe DFUs. After adjusting for baseline differences, beneficiaries receiving PCMP* had lower rates of amputations, and lower costs for hospitalization and skilled nursing facility visits than those not receiving PCMP*.

.png)